The recent voluntary commitments from the nation's leading health plans mark a watershed moment in healthcare — an inflection point where bold action meets systemic need. Anterior, a healthcare-native clinical AI platform, stands ready to help health plans turn these commitments into real-world impact. Below, we detail the dynamics prompting these transformative changes, outline core solution requirements for achieving the goals, and share exactly how our technology supports each pillar of the commitment — from real-time decisioning to continuity of care and clinician-in-the-loop oversight.
The AHIP commitment
Recently, a group of health insurance plans, alongside AHIP and the BlueCross BlueShield Association, came together to announce their voluntary commitment to make healthcare “safer, more effective, and more affordable.” This type of collective action is an acknowledgment that the status quo needs to shift and marks a step toward meaningful change that will impact millions of patients.
Specifically, the commitment highlights areas of focus within the Utilization Management (UM) function of health plans, and puts forth a vision for a more seamless, tech-enabled experience for patients, providers, and plans.
Why is this important?
Anterior recognizes the vital role that health plans play in stewarding resources across the healthcare system, enforcing quality of care standards, and providing the financial infrastructure to effectively administer care across an ever increasingly expansive scope of care.
Utilization Management is one part of a larger system designed to guide members to the right care, at the right time, with the right provider. But today, that system is under immense pressure.
Across the board, health plans are seeing fewer members entering their plans, while the cost of care continues to rise. This imbalance creates a ripple effect: fewer premiums coming in, more dollars going out, and increasing pressure on payers, providers, and ultimately, patients.
The sustainability of our current healthcare system is at stake and everyone is affected.
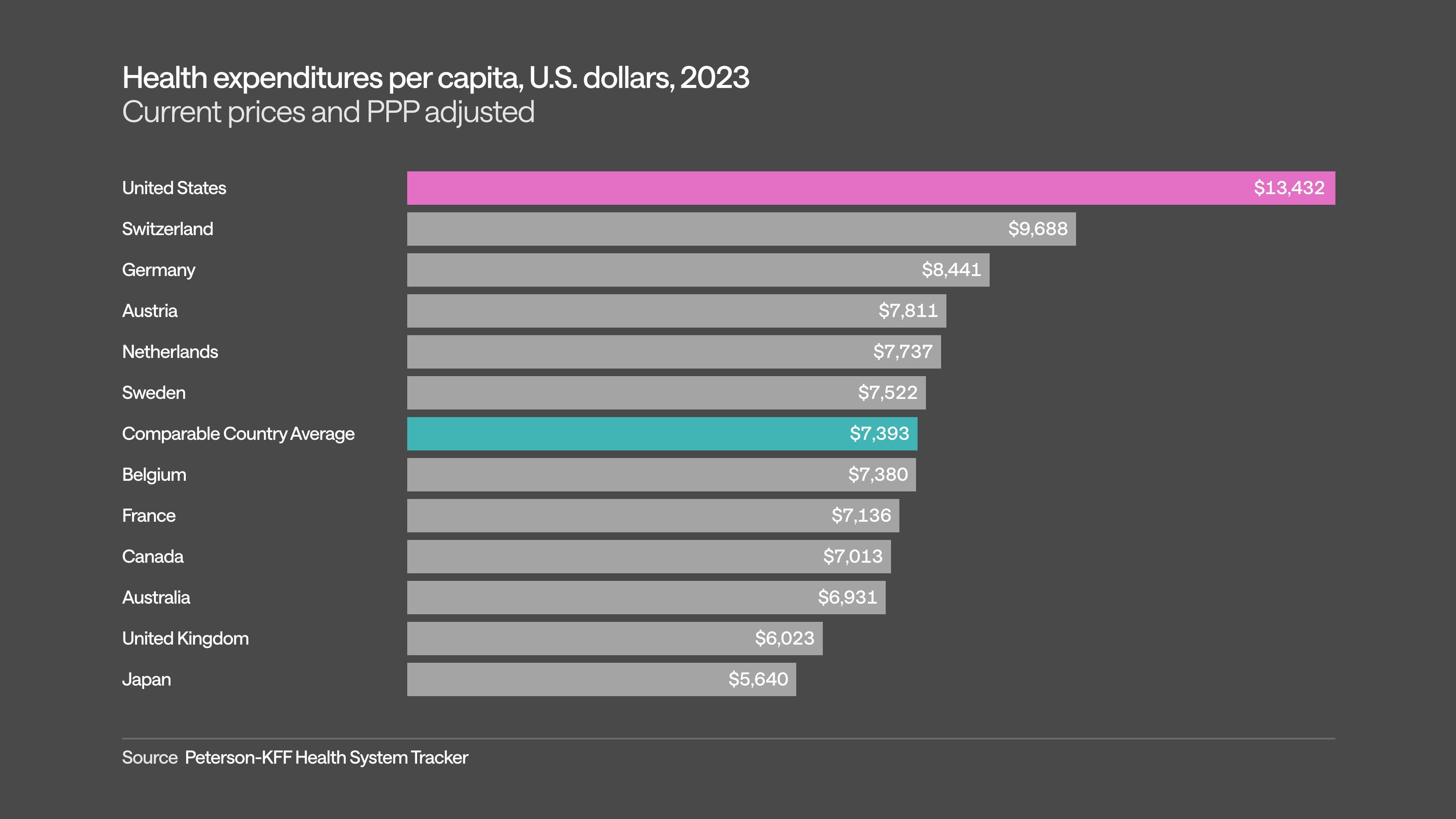
In the US, we spend more per person on healthcare than any other high-income nation. At the same time, these outsized costs fail to deliver consistent improvements in quality outcomes for patients. A significant portion of cost stems from fragmented care delivery, data silos, adverse provider incentives, and legacy infrastructure that undermines standards of care, makes care harder to coordinate and harder to afford.
Health plans use Utilization Management processes to both reinforce standards of care and combat waste, fraud, and abuse perpetuated by fragmentation and poor infrastructure.
But current UM processes are too burdensome for plans, providers, and patients, and fail to sufficiently steward system resources. As health plans operate under financial strain, it doesn’t just affect their balance sheets — it affects access and outcomes for patients. Unsustainable premium-to-cost dynamics lead to plan exits from markets which lead to narrower options for coverage, less diversity of care options, and further increases in cost.
Prior authorization is the place to start
Prior authorization, one notable aspect of broader UM practices, has rightfully become a flashpoint in the healthcare stewardship conversation. For patients and providers, it can be a source of frustration and delay. While designed to ensure appropriate, high-value care, the current prior auth process often leads to unintended consequences: delayed treatments, redundant appointments, and growing administrative burden.
But it’s important to acknowledge that prior authorization exists for a reason. At its best, it’s a tool to help ensure that members receive safe, effective, and necessary care that is aligned with the latest clinical evidence. It also directly combats drivers of rising costs from provider silos to perverse behaviors.
The goal isn’t to block care — it’s to guide it and sustainably pay for it.
That’s why reforming prior authorization is one of the clearest ways to meaningfully reduce burden and improve health outcomes.
So what’s the solution?
In response to the increasing complexity of the system, the healthcare industry turned to digitization and automation to bring scale and consistency to processes like billing, documentation, and utilization review. These rule-based solutions have played a critical role in structuring healthcare data and standardizing operations. But by design, they operate on fixed logic — hardcoded rules that, while effective in many contexts, can’t flex to accommodate clinical nuance, policy variation, or evolving medical knowledge.
For the first time ever, we are seeing a paradigm shift with the massive adoption of large language models (LLM) and artificial intelligence (AI). Instead of static rules, AI enables systems that learn from data and adapt dynamically to new inputs. This unlocks a fundamentally different kind of intelligence that can reason across unstructured clinical notes, adjust decisions in real time, and personalize outputs based on context. In this way, AI doesn’t replace past solutions — it extends them, offering a path toward more responsive, scalable, and human-centered healthcare. This is a time where “everything's starting to line up; payers, technology companies, the regulators, non-industry stakeholders [and it feels like a] strike-while-the-iron's-hot type of thing,” said a health plan executive we spoke to recently.
Below are specific ways Anterior is committed to helping every Signatory Plan achieve their prior auth commitments:
Standardizing Electronic Prior Authorization
Commitment: Signatory Plans will work toward the development and implementation of common, transparent submissions for electronic prior authorization. This commitment includes the development of standardized data and submission elements (using FHIR® APIs) that will support seamless, streamlined processes and faster turn-around times.
At Anterior, we strongly support the industry’s move toward standardized and transparent electronic prior authorizations. Clinicians at plans and care delivery orgs should not be burdened with fragmented, manual processes when technology can support a faster, more transparent path to care.
As a healthcare-native clinical AI platform, Anterior is already building for this future:
- FHIR-native Infrastructure: Our platform is built to natively support FHIR® APIs, enabling structured, interoperable data exchange between payers and providers. We believe FHIR is not just a checkbox, but a foundation for real-time, context-aware decisions.
- Backwards interoperability: Our schema-first data approach paired with a comprehensive set of adapters supports legacy interoperability standards and seamless interactions between FHIR and X12 EDI, SOAP, SFTP batch, and fax data formats.
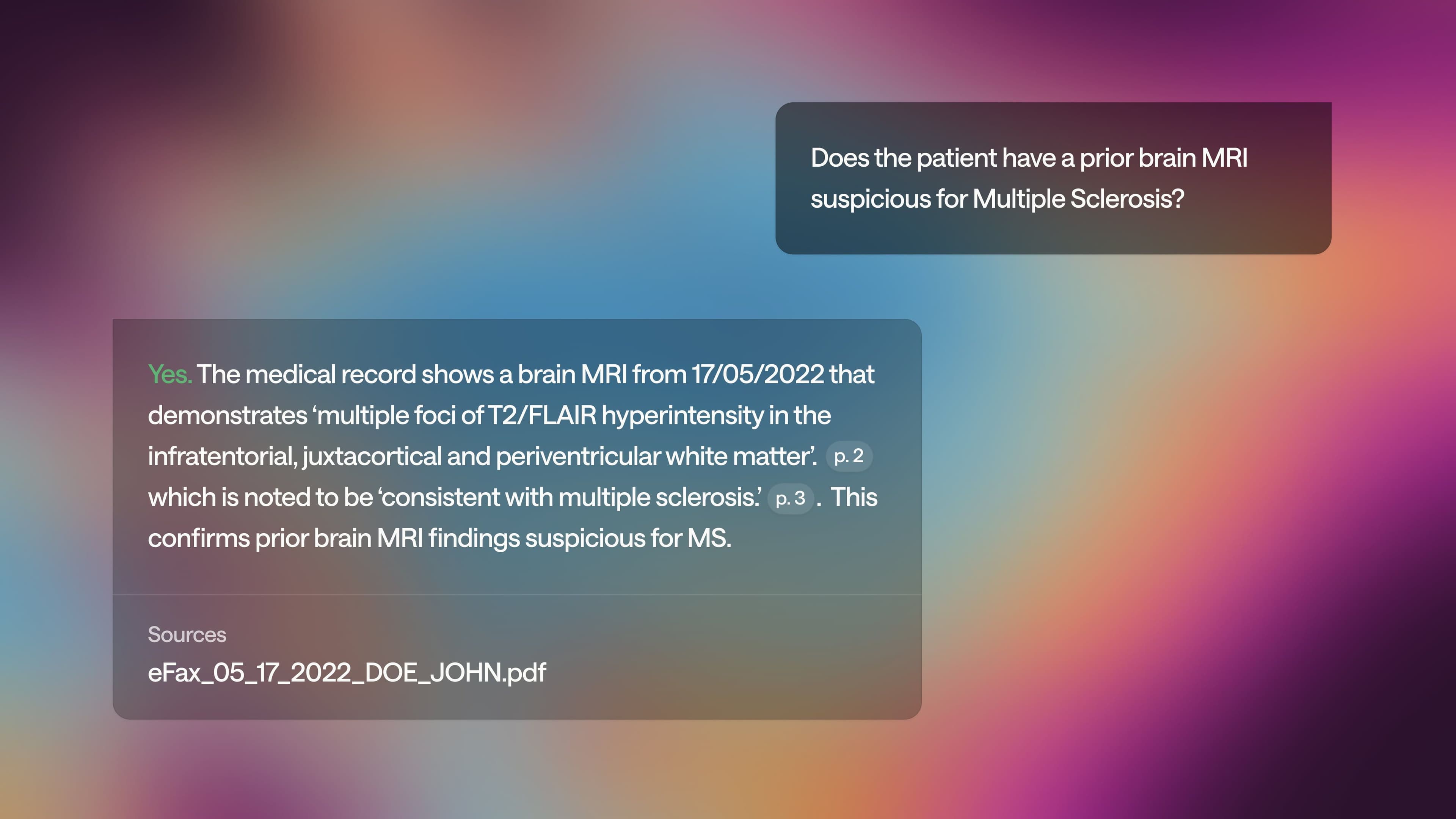
- Clinical intelligence: Data and submission standardization alone isn't enough. The submission process must also reflect the clinical nuance of each patient. Our platform uses clinical reasoning paired with LLMs to extract relevant information directly from clinical documentation — automatically populating prior auth submissions with the patient-specific context plans need.
- Accelerating decision timeframes: With both standardized formats and intelligent extraction, we enable prior auth submissions that are more complete, reducing back-and-forth and driving faster determinations for patients and providers alike.
We believe the industry’s shift toward standardized, electronic prior authorization is necessary and achievable. But to truly transform the experience, we must go beyond structure and focus on clinical context, data usability in the form of LLM-readiness, and accurate, evidenced clinical reasoning.
Reducing the Scope of Claims Subject to Prior Authorization
Commitment: Signatory Plans providing fully insured, ACA marketplace coverage and Medicare Advantage coverage commit that they will individually reduce the volume of in-network medical prior authorizations by January 1, 2026. Signatory Plans further commit that they will provide data to allow industry reporting of the extent of such reductions reflecting actions taken since January 2024.
At Anterior, we believe the industry is long overdue for a smarter, more targeted approach to prior authorization — one that reserves oversight for true clinical complexity, not routine care.
While policy decisions around prior authorization requirements lie with each payer, we see our role as enabling the shift: making it easier, safer, and more data-driven to reduce the volume of low-value or unnecessary auths.
Here’s how:
- Data-driven de-escalation: Our platform gives payers deep visibility into prior auth patterns — highlighting low-denial, low-variation services that may no longer need authorization. We help build the case for safe removal, backed by real-world data.
- Provider insights at scale: Prior authorization should focus on nuance, not noise. Our clinical reasoning helps payers evolve toward a model that’s more selective and informed by historical and real-time trends in provider insights.
As payers commit to reducing the scope of prior authorization, Anterior provides the intelligence layer that makes that reduction safe, sustainable, and clinically sound.
Ensuring Continuity of Care When Patients Change Health Plans
Commitment: By January 1, 2026, Signatory Plans commit to support continuity of care by honoring a previous health plan’s prior authorization for the same service, under the same type of benefit in network for a 90-day transition period when a member changes health plans after starting a course of treatment.
We believe continuity of care shouldn’t break just because a patient changes health plans and we’re excited to see this commitment. While it's up to health plans to honor prior authorizations during transitions, Anterior can play a key role in making that continuity technically and clinically possible.
Here’s how we help:
- Structured, interoperable prior auth data: Our platform captures prior authorization decisions in standardized, structured formats — making it easier for health plans to share, ingest, and recognize previously approved services, even when data comes from another plan.
- FHIR-native architecture: Anterior is built on FHIR® standards, which are critical for seamless exchange of prior auth data across plan transitions.
- Clinical traceability: We ensure that prior auth decisions are traceable to the actual originating clinical documentation, not just summaries or codes, giving receiving plans confidence in the transferred authorization and that the service was medically necessary and appropriately approved.
- Provider-friendly resubmissions (when needed): In cases where reauthorization is required, we minimize disruption by allowing providers to re-submit with minimal friction — automatically extracting relevant clinical data from the EMR, unstructured clinical documentation (including PDFs and handwritten notes), and the transferring plan's UM portal to avoid repeating paperwork.
Continuity of care shouldn’t depend on more paperwork. We’re building the infrastructure that helps payers make continuity a reality — so patients don’t fall through the cracks during transitions.
Enhancing Communication and Transparency on Determinations
Commitment: By January 1, 2026, for fully insured and self-insured Commercial coverage and ACA marketplace coverage, Signatory Plans commit to explaining with clear and personalized language about any prior authorization denials, including information about next steps and available appeals processes. Signatory Plans also will explore seeking regulatory changes to facilitate expansion of this commitment. Signatory Plans serving Medicare Advantage beneficiaries will work with CMS to improve existing mandatory member communications on prior authorization denials and appeals.
Commitment: By January 1, 2026, for fully insured and self-insured Commercial coverage and ACA marketplace coverage, Signatory Plans commit to providing staff to help members understand the prior authorization process and their options after a prior authorization determination is made.
We support this industry commitment and play a direct role in making it easier for plans to fulfill it both efficiently and at scale.
Here’s how Anterior helps:
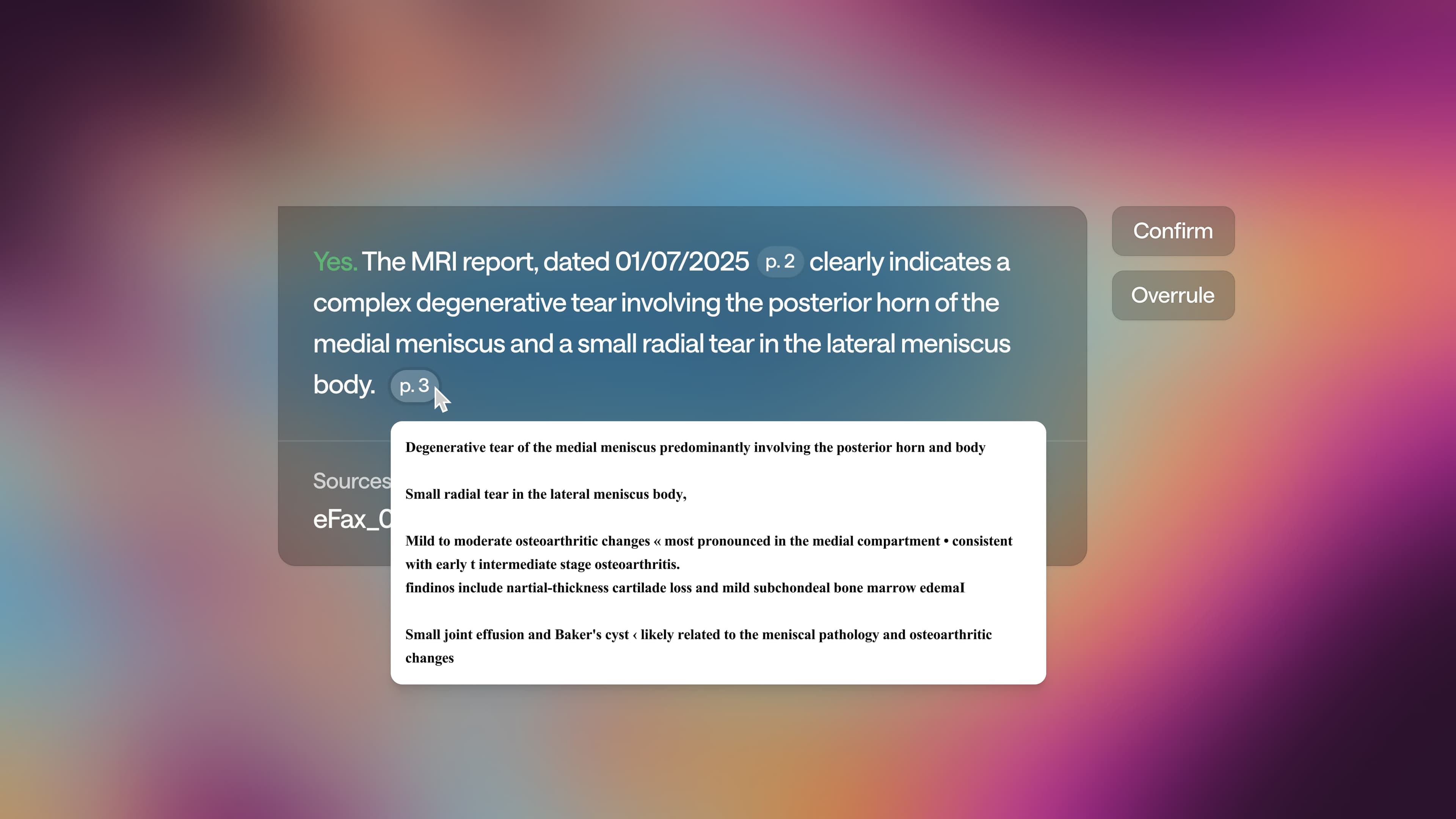
- Human-in-the-loop and auditability: Rather than offering prior auth recommendations as a black box, Anterior facilitates automated and human-in-the-loop reviews that provide full explainability and auditability. Patient care is never delayed and all denials are determined by qualified human clinicians. Health plans are given all the tools and information needed to show the exact reason for determination in member approvals or denials communications. Our AI reasoning finds every possible path towards approval and shows a logical, step-by-step process for that path, unlike other black box solutions. Every step-level recommendation or determination in the path has a full chain of reasoning and cited evidence.
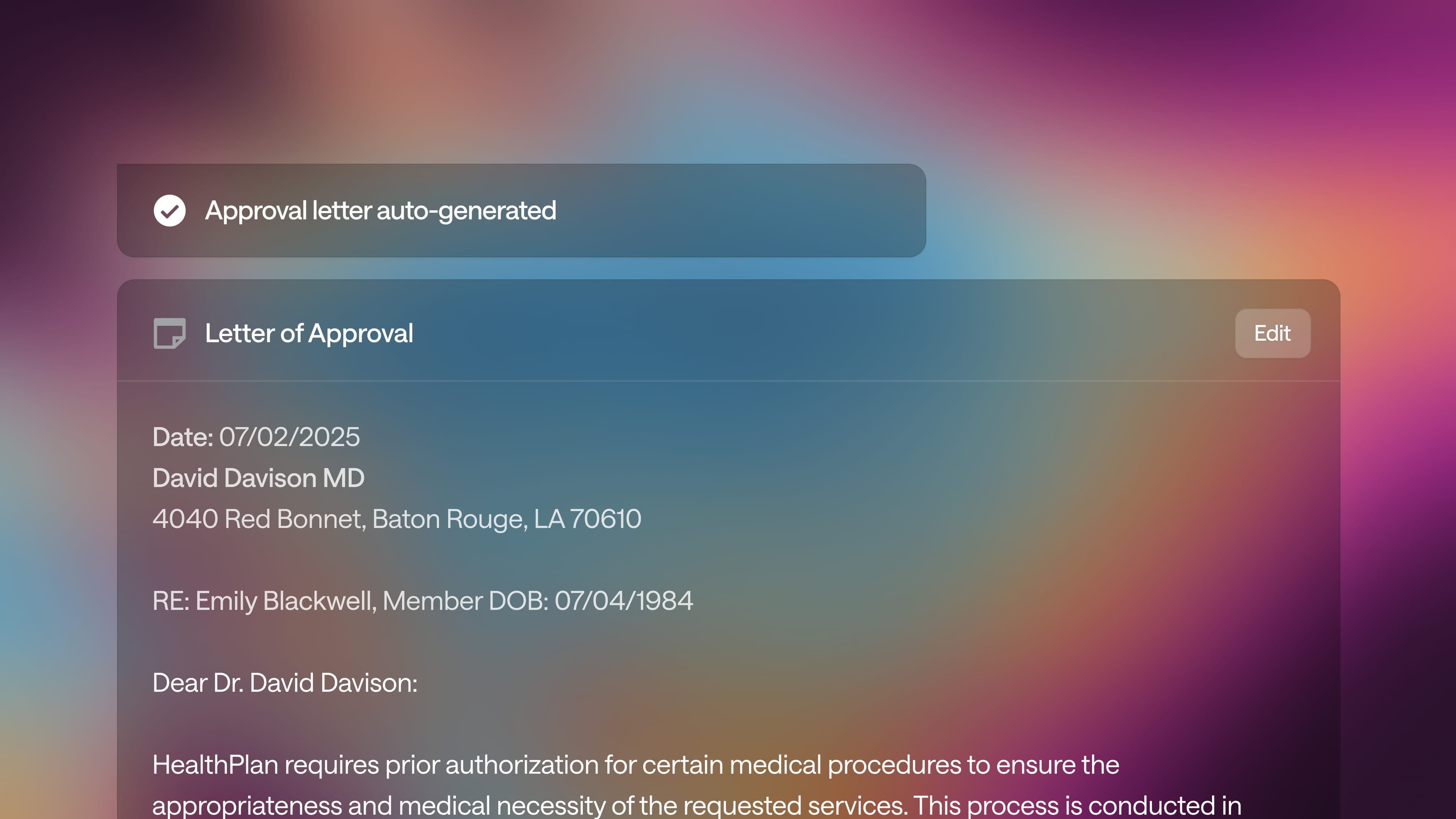
- Standardization and consistency: Once a determination has been reached, our platform enables plans to generate denial and approval notices using standardized templates that are customizable to meet plan-specific language, regulatory requirements, and tone, and personalized based on member-specific details of each determination — ensuring both consistency and personalization, without sacrificing clarity.
With structured clinical summaries and plain-language decision context, our platform makes it easier for payer staff to communicate clearly with members who need help navigating next steps.
Expanding Real-Time Responses
Commitment: Signatory Plans commit to an acceleration of the percentage of prior authorization requests for medical services answered in real-time if submitted electronically by providers with all necessary clinical documentation. By 2027, for all coverage types at least 80% of prior authorization approvals will be answered in real-time.
Commitment: While existing regulations require new technical standards for electronic prior authorization for certain health plans in federal programs beginning January 1, 2027, health plans subject to these forthcoming rules will support these standards (FHIR® APIs) for all lines of business.
To achieve real-time approvals for 80% of prior auths, plans need to leverage both automated approval workflows which leverage AI reasoning to make high confidence determinations without loss of explainability and auditability, and human-led reviews which are powered by co-pilot technologies to audit automated decisions and handle escalations. Together, these approaches accelerate and improve accuracy of decision making while getting the vast majority of decisions to real-time answers.
Here’s how Anterior helps:
- More auto-approvals: LLM-powered automated approval workflows can handle most low and medium complexity cases and plans are already leveraging Anterior to do so. Anterior’s automated medical necessity reviews are proven to reduce prior auth approvals needing human review by ~76%. This reduction is due to our ability to ingest payer rulesets, policies, and guidelines, ingest unstructured member clinical data, and to layer our AI clinical reasoning over it all to provide an approval path. With this technology, our platform is fully ready to take on the challenge of near real-time approvals of 80% of electronic prior authorization requests for medical services.
- Increased accuracy: While speed is of great importance, Anterior is even more proud of our ability to reduce the margin of error with the approvals moved into auto-approval with 99.26% accuracy. Compared to human accuracy of 86%, it stands to reason that increasing speed of approvals with Anterior comes hand-in-hand with more accurate approvals.
Ensuring Medical Review of Non-Approved Requests
Commitment: For all coverage types, Signatory Plans commit that all prior authorization denials based on medical necessity for clinical factors will be reviewed by a licensed and qualified clinician. This commitment reflects existing practices and is in effect now.
Anterior also provides powerful tools to support prior authorizations requiring escalation to humans.
- Responsible, positive outcomes: Our platform is designed to find all possible paths to approval and cannot deny, delay, or modify a patient’s care. If there is any uncertainty and/or a path to approval can’t be found, the decision is always escalated to a human for review, also known as human-in-the-loop. Clinicians are always empowered to make the final determination after validating, correcting, or overriding the AI reasoning.
The key here is our platform supports clinicians with reducing wasted time reading through complicated clinical documentation, chasing down phone trees, and more. With Anterior’s side-by-side guidance, complex escalated cases take clinicians 74% less time to come to a decision.
A toolkit to success
AI has emerged as an unprecedented game changer, particularly when applied to streamlining prior authorization. And yet, there’s understandable skepticism. In a recent survey, 61% of physicians surveyed report that they are concerned AI will increase denial rates in prior authorization processes.
But AI doesn’t have to be a black box. And it certainly doesn’t have to replace clinical expertise. We're already seeing rapid AI adoption in a plethora of other clinical encounters. According to recent AMA survey, 2 in 3 physicians are using an AI in their practice, ranging from documentation of visit notes; creation of discharge instructions, care plans or progress notes; translation services, assistive diagnosis and more. And 35% of physicians already reported that their enthusiasm for health AI exceeded their concerns.
The real opportunity lies in human-centered AI; systems designed with clinicians, for clinicians, and technology that enhances, not overrides, medical judgment. When used appropriately, AI can help automate the administrative lift, flag exceptions, and prioritize cases that truly need clinician oversight. The result? Faster decisions, better outcomes, and a system that works smarter for everyone involved.
In the coming days, Anterior will be releasing a comprehensive UM Transformation Playbook that will lay out the key steps towards integrating any AI solution into existing tech stacks.
Want to get notified of the playbook release?